One of the most anticipated features that agencies look for in a new EHR software is efficient and accurate billing. The potential time savings and improved revenue flows that come with streamlined billing processes are highly sought after, and can revolutionize the way agencies do business .
A well-designed EHR billing software is essential in reducing the time and expenses associated with billing. It not only provides agencies with a means to enhance the accuracy of their billing processes, but also mitigates the risks of billing errors, and helps agencies get reimbursed faster.
Exym's EHR Billing Software Process: Before Claims Are Submitted
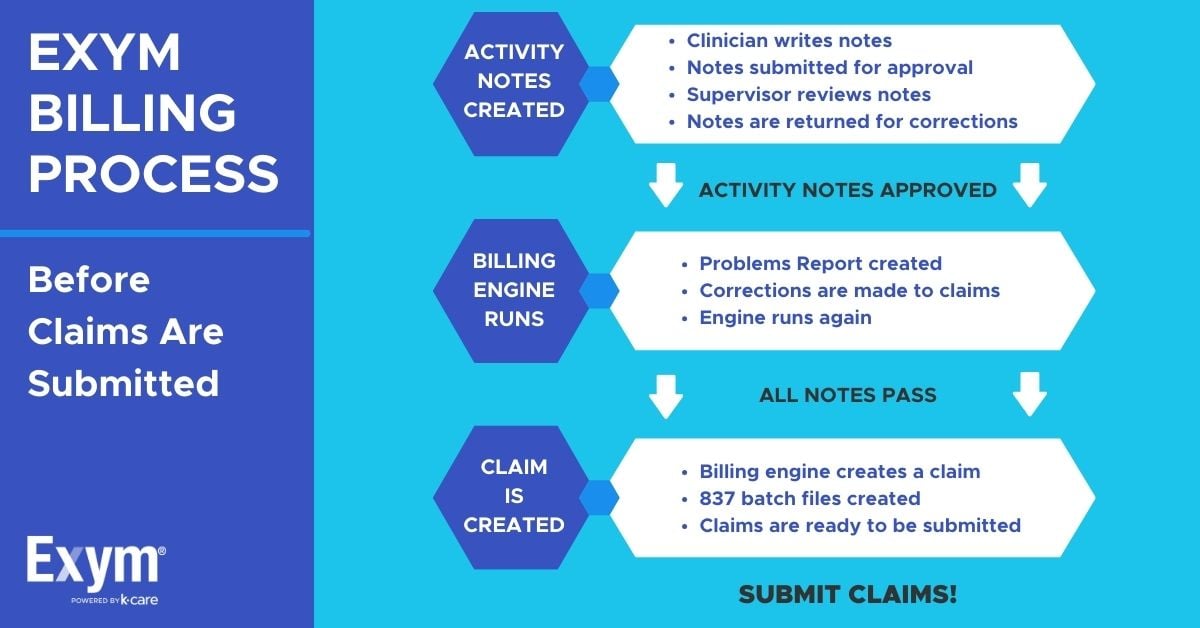
Before a billing claim is created, Exym's EHR billing software runs hundreds of checks to make sure the claim is correct and ready for submission. When an activity note is first created, it is scanned by the billing software to:
- Ensure the client is set up for billing
- Discover any relevant contracts
- Obtain notes approval
- Look for age restrictions
- Note any other demographic data
- Make sure the provider and agency have an NPI number
The EHR billing software will run checks that are general to all agencies, as well as specific customized checks that may be relevant for a particular agency or specific provider. Agencies can also create even more additional checks if needed, so nothing slips through the cracks.
If there are claims with issues, a “Claims with Problems” report is created so they can be addressed before the claim is submitted. After corrections are made, the engine runs again and will keep flagging errors until the claim is 100% ready for submission.
Exym's EHR Billing Process: After Claims Are Submitted
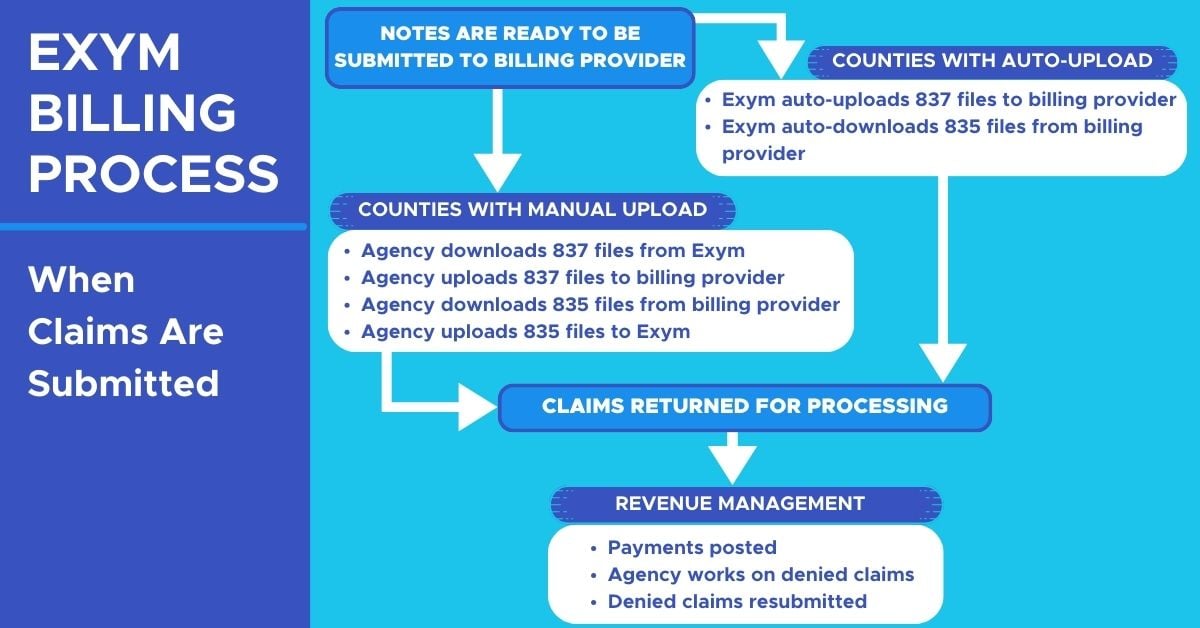
After a claim is created and verified it is ready to be submitted to the billing provider. For counties that support an auto-upload feature, Exym's EHR billing software auto-uploads the claims to the billing provider. For counties without the auto-upload feature, agencies upload their 837 files to the billing provider themselves. Once claims are uploaded, payments can post and denied claims are flagged. Agencies can then correct denied claims and resubmit them for payment.
What do Exym Customers Have to Say About EHR Billing?
One of our satisfied customers, Kristin Santoro from Didi Hirsch, has shared her positive experience with Exym billing software.
“If you are contracted through Department of Mental Health, Exym is hands-down the best EHR to go with. They stay on top of the DMH and state regulations and are sure to be in compliance every step of the way.”
-Kristin Santoro, Vice President of Quality and Innovation at Didi Hirsch
Exym's Behavioral Health EHR Software Saves Time and Optimizes Revenue
Are you looking for a more robust EHR billing software that is tailored to your needs?
Exym is a comprehensive EHR software solution designed specifically for behavioral health agencies. Trusted for 20+ years, our intuitive and customizable software empowers providers to improve client outcomes, manage revenue cycles, and increase agency efficiency. Exym allows you to spend more time on what matters most- the clients in your care.
It’s never too late to switch to an EHR billing software that better suits your needs! We invite you to learn more about Exym's billing features on our Finance Page, or book a demo with an Exym expert so they can answer your questions and help you get started.
Tags:
Finance
February 21, 2021


.jpg?width=1200&height=628&name=Exym-Behavioral-Health-EHR-Software%20(1).jpg)


Comments